The United States healthcare system is notorious for burdening patients with hefty expenses — a reality that existed long before the COVID-19 pandemic turned a national spotlight onto the issue.
Financially-strained consumers can struggle to afford medicine and treatment for a variety of conditions, and some skip on getting the care they need simply because it is too expensive. Patients with rare conditions can be confronted with costs of up to $2.1 million for a full course of treatment, and even the average consumer spent $1,200 on prescription medicine during 2018.
Patients’ financial plight is both a humanitarian issue and a business one, with the healthcare system unable to get revenue if customers are unable to pay. Pharmacies lose money if consumers and their insurance companies cannot meet their prices, for example — a reality that has spurred many drug manufacturers to offer partial reimbursements to help soften the impact of their high prices.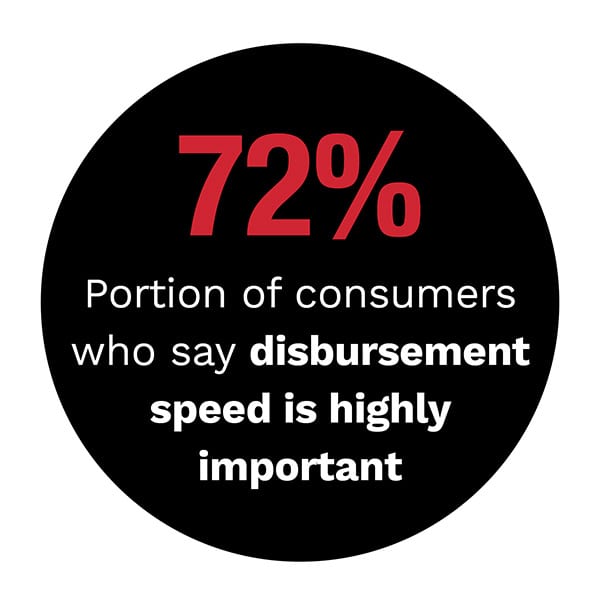
Consumers can also expect reimbursements from insurance companies that overcharge them or required them to pay upfront for covered expenses, as well as from hospitals in cases of accidental overbilling. These funds need to arrive quickly, or patients may face serious financial strains during their wait. Consumers’ utility bills do not go on hold just because reimbursements are slow arriving, after all. Paper checks sent by mail therefore may not be enough to support consumers in need.
The Faster Healthcare Payments Report, in collaboration with Mastercard, examines the issues that slow down patient reimbursements as well as how payment modernizations can ease some of these pains.
Advertisement: Scroll to Continue
How Streamlining MLR Rebates Can Keep Insurance Policyholders Loyal
Consumers have some financial protections on their side against the high costs of healthcare. The Affordable Care Act’s (ACA) medical loss ratio (MLR) provision is one tool, and it requires health insurance companies to refund  policyholders if they overcharge them on premium prices. Some of these refunds never reach policyholders, however, with $38 million worth of rebates going unclaimed between 2012 and 2019. Rebates sent via paper check may get lost in the mail or fail to be redirected to recipients’ new addresses. Digital disbursement methods might ease those frictions.
policyholders if they overcharge them on premium prices. Some of these refunds never reach policyholders, however, with $38 million worth of rebates going unclaimed between 2012 and 2019. Rebates sent via paper check may get lost in the mail or fail to be redirected to recipients’ new addresses. Digital disbursement methods might ease those frictions.
We’d love to be your preferred source for news.
Please add us to your preferred sources list so our news, data and interviews show up in your feed. Thanks!
Check out the Report’s Case Study to learn more.
Understanding Patients’ Payment Pains
U.S. consumers often wait weeks before they receive compensation for being overcharged by insurance carriers or hospitals. This is an especially troubling situation when considered against the fact that lack of even $23 for transportation can prevent patients from getting to their medical appointments, according to Caitlin Donovan, senior director of public relations for patient financial assistance and advocacy organizations the National Patient Advocate Foundation and the Patient Advocate Foundation.
Board-certified patient advocate (BCPA) Bonnie Sheeren of Houston Health Advocacy, and Steven Corn, BPCA at Metis Advocacy, also spoke with PYMNTS about patients’ struggles with being overbilled and the frictions that can hold up compensation.
Find the Feature Story in the Report.
Deep Dive: Modernizing Patient’s Reimbursements, Discounts
Paper-based disbursements sent in the mail are often slow to reach patients. This delay is both a problem for the consumers and for their healthcare providers because patients who are waiting for funds may then be unable to pay their caregivers in a timely manner. Hospitals, insurance companies and medical providers have been exploring how greater digitization can accelerate patient reimbursements and improve payment flows throughout the sector. The Deep Dive examines the factors that slow down healthcare industry payments as well as strategies being considered for overcoming them.
providers because patients who are waiting for funds may then be unable to pay their caregivers in a timely manner. Hospitals, insurance companies and medical providers have been exploring how greater digitization can accelerate patient reimbursements and improve payment flows throughout the sector. The Deep Dive examines the factors that slow down healthcare industry payments as well as strategies being considered for overcoming them.
Download the Report to get the full story.
How Push Payments Could Cure Healthcare Frictions
Some players in the payments space believe that disbursements can be accelerated if they are sent via digital methods rather than paper checks. In the Report’s Executive Perspective, Mastercard senior vice president of digital payments Silvana Hernandez discusses where digital push payment methods could ease payment flows for the healthcare space as well as the barriers that have prevented their widespread adoption.
Read more in the Report.
About The Report
The Faster Healthcare Payments Report, done in collaboration with Mastercard, details the slow state of patient reimbursements.

